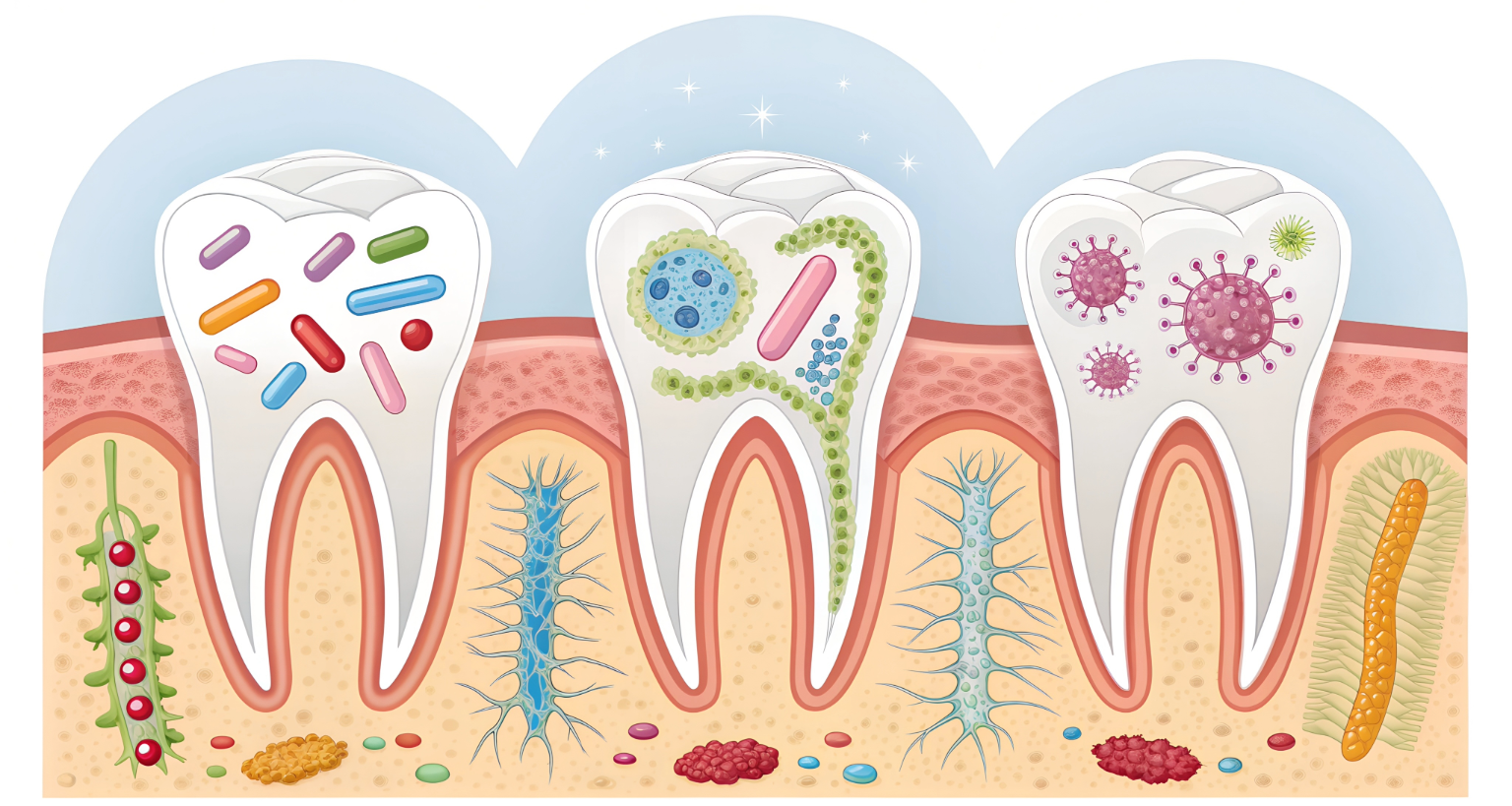
Your mouth serves as the gateway to your entire body, harboring over 700 different species of bacteria. While many people view oral health as separate from overall wellness, emerging research reveals a startling truth: the state of your mouth directly influences your systemic health. Understanding how oral bacteria affect the body can transform your approach to daily hygiene and potentially prevent serious chronic diseases.
Poor oral hygiene creates a breeding ground for harmful bacteria that don’t stay confined to your mouth. These pathogens can enter your bloodstream, trigger widespread inflammation, and contribute to conditions ranging from heart disease to diabetes. The mouth-body connection represents one of the most significant yet overlooked aspects of preventive healthcare.
This comprehensive guide explores the complex relationship between oral infections, chronic inflammation, and systemic health while examining how conventional oral hygiene products may unknowingly contribute to these problems.
Understanding Common Oral Infections
Oral infections begin when harmful bacteria overwhelm the natural balance in your mouth. The most prevalent types include dental caries (cavities), gingivitis, and periodontitis, each representing different stages of bacterial colonization and tissue destruction.
- Dental caries develop when acid-producing bacteria like Streptococcus mutans metabolize dietary sugars, creating an acidic environment that demineralizes tooth enamel. Left untreated, these infections can penetrate deeper into the tooth structure, potentially reaching the pulp and creating abscesses.
- Gingivitis occurs when bacterial plaque accumulates along the gumline, causing inflammation, bleeding, and swelling of the gingival tissues. This condition affects nearly 50% of adults and often progresses silently without proper intervention.
- Periodontitis represents the advanced stage of gum disease, where bacterial toxins and inflammatory responses destroy the tissues and bone supporting your teeth. This irreversible condition affects approximately 42% of adults over 30 and creates deep pockets where dangerous bacteria can thrive.
Several factors increase your risk of developing oral infections, including poor oral hygiene, frequent sugar consumption, dry mouth conditions, smoking, hormonal changes, certain medications, and genetic predisposition. Stress also plays a significant role by suppressing immune function and promoting bacterial growth.
The Science of Chronic Inflammation
When oral bacteria establish infections, your immune system launches an inflammatory response designed to eliminate the threat. However, persistent bacterial presence transforms this protective mechanism into chronic inflammation, creating a continuous cycle of tissue damage and repair attempts.
The body’s inflammatory response involves releasing chemical mediators like cytokines, prostaglandins, and inflammatory enzymes. These substances increase blood flow, cause tissue swelling, and recruit immune cells to the infected area. While acute inflammation helps fight infections, chronic inflammation becomes destructive to both oral and systemic tissues.
Research demonstrates that gum disease and systemic inflammation share common pathways. Inflammatory markers like C-reactive protein (CRP), interleukin-6, and tumor necrosis factor-alpha become elevated in both conditions, suggesting that oral infections contribute to body-wide inflammatory burden.
The concept of biological dentistry inflammation emphasizes how oral health directly impacts systemic inflammatory processes, highlighting the need for comprehensive approaches to oral care that support rather than disrupt the body’s natural healing mechanisms.
Critical Links to Systemic Health
Cardiovascular Disease
The connection between dental infections and heart disease represents one of the most well-documented examples of how oral bacteria affect the body. Periodontal pathogens like Porphyromonas gingivalis can directly invade coronary arteries, contributing to atherosclerotic plaque formation and increasing cardiovascular event risk.
Studies show that individuals with severe gum disease have a 2-3 times higher risk of heart attack and stroke. The inflammatory cytokines produced in response to oral infections promote endothelial dysfunction, blood clot formation, and arterial narrowing. Additionally, oral bacteria entering the bloodstream can directly colonize heart valves, particularly in individuals with existing cardiac conditions.
Diabetes and Blood Sugar Control
Gum disease and systemic inflammation create a bidirectional relationship with diabetes that significantly impacts blood sugar control. Chronic oral infections increase insulin resistance, making diabetes management more challenging and potentially accelerating the development of diabetic complications.
Diabetic individuals face increased susceptibility to gum disease due to compromised immune function and altered wound healing. This creates a vicious cycle where poor oral health worsens diabetes, and uncontrolled diabetes further deteriorates oral health. Research indicates that treating gum disease can improve glycemic control and reduce inflammatory markers in diabetic patients.
Respiratory Health
The mouth serves as a reservoir for respiratory pathogens that can be aspirated into the lungs, particularly in elderly or immunocompromised individuals. Pneumonia-causing bacteria like Streptococcus pneumoniae and Haemophilus influenzae frequently colonize the oral cavity before causing lower respiratory tract infections.
Poor oral hygiene and health risks extend to chronic obstructive pulmonary disease (COPD) and other respiratory conditions. Inflammatory mediators from oral infections can exacerbate existing lung inflammation and impair respiratory function. Maintaining optimal oral health becomes crucial for individuals with compromised respiratory systems.
Additional Health Connections
Emerging research reveals connections between oral health and pregnancy outcomes, with gum disease linked to preterm birth and low birth weight. Rheumatoid arthritis shares inflammatory pathways with periodontal disease, and some studies suggest oral bacteria may trigger autoimmune responses in susceptible individuals.
Cognitive health may also be affected, as oral bacteria have been detected in brain tissue of Alzheimer’s patients, suggesting a potential role in neurodegenerative processes. The mouth-body connection continues to reveal new pathways through which oral health influences systemic wellness.
The Hidden Dangers in Conventional Oral Care Products
Most commercial toothpastes and mouthwashes contain synthetic chemicals that may disrupt oral microbiome balance and contribute to systemic health problems. Understanding these toxic elements helps explain why many people continue experiencing oral health issues despite regular brushing and flossing.
- Fluoride, while promoted for cavity prevention, raises concerns about systemic toxicity, particularly with chronic exposure. Research suggests fluoride accumulation in body tissues may interfere with thyroid function, bone health, and neurological development. Many countries have reduced or eliminated water fluoridation due to these safety concerns.
- Sodium Lauryl Sulfate (SLS) creates the foaming action in most toothpastes but can cause oral irritation, canker sores, and disruption of beneficial bacteria. This harsh detergent strips away the mouth’s natural protective barriers, potentially increasing susceptibility to infections.
- Artificial preservatives, colors, and sweeteners in conventional oral care products provide no health benefits while potentially contributing to allergic reactions, hormonal disruption, and microbiome imbalances. These synthetic additives accumulate in body tissues over time with unknown long-term consequences.
- Antimicrobial agents in mouthwashes, while killing harmful bacteria, also eliminate beneficial microorganisms essential for oral health. This disruption can lead to dysbiosis, where pathogenic bacteria proliferate after beneficial species are destroyed.

The Biological Approach: ROZE BioHealth Products
Biological dentistry recognizes that oral health products should support the body’s natural healing mechanisms rather than introducing potentially harmful chemicals. ROZE BioHealth represents a revolutionary approach to oral care, formulated by dentists who understand the critical importance of biocompatible ingredients.
- Hydroxyapatite forms the foundation of ROZE BioHealth toothpastes, comprising 15% of each formula. This naturally occurring mineral makes up 97% of tooth enamel and has been proven to remineralize teeth, reduce sensitivity, and provide superior protection without the risks associated with fluoride. Originally developed by NASA for astronauts, hydroxyapatite has been used successfully in Japanese oral care for over 40 years.
- 100% Natural Ingredients ensure that every component serves a beneficial purpose without introducing toxins. The carefully selected botanical extracts, essential oils, and minerals work synergistically to clean teeth, support gum health, and maintain optimal oral pH balance.
- Toxin-Free Formulation means complete elimination of fluoride, SLS, preservatives, artificial colors, and synthetic sweeteners. This approach prevents the accumulation of harmful substances while supporting the mouth’s natural microbiome balance.
- Dentist-Formulated Products reflect deep understanding of oral physiology and the mouth-body connection. ROZE BioHealth products are created by practicing dentists who recognize that oral care should enhance rather than compromise systemic health.
ROZE BioHealth’s commitment extends beyond ingredients to sustainable practices, including biodegradable bamboo toothbrushes and eco-friendly packaging. This holistic approach recognizes that environmental health directly impacts human health.
Comprehensive Prevention and Treatment Strategies
Preventing oral infections and chronic disease requires a multifaceted approach that addresses diet, hygiene practices, professional care, and product selection. Understanding how oral bacteria affect the body empowers you to make informed decisions about your daily oral care routine.
- Effective Daily Hygiene should include gentle brushing with biological toothpaste, regular flossing or interdental cleaning, tongue scraping to remove bacterial biofilm, and rinsing with pH-balancing solutions. Timing matters—avoiding brushing immediately after acidic foods or drinks prevents enamel damage during vulnerable periods.
- Nutritional Support plays a crucial role in oral health, with emphasis on reducing refined sugars that feed harmful bacteria, increasing antioxidant-rich foods that support immune function, ensuring adequate vitamin D and K2 for bone and tooth health, and staying properly hydrated to maintain saliva production.
- Professional Care should include regular dental examinations and cleanings, early intervention for developing problems, and consideration of biological dentistry approaches that prioritize biocompatible materials and conservative treatments.
- Lifestyle Modifications such as stress management, smoking cessation, limiting alcohol consumption, and addressing underlying health conditions contribute significantly to oral health outcomes and overall inflammatory burden reduction.
Taking Action for Your Health
The evidence clearly demonstrates that oral health cannot be separated from systemic wellness. How oral bacteria affect the body extends far beyond tooth decay and gum disease, influencing your risk for cardiovascular disease, diabetes, respiratory infections, and other chronic conditions.
Choosing biological oral care products represents a simple yet powerful step toward reducing your toxic burden while supporting optimal oral health. ROZE BioHealth offers scientifically-formulated solutions that work with your body’s natural processes rather than against them.
The mouth-body connection demands a comprehensive approach to healthcare that recognizes oral health as fundamental to overall wellness. By understanding the links between dental infections and heart disease, gum disease and systemic inflammation, and poor oral hygiene and health risks, you can make informed decisions that protect both your oral and systemic health.
Consider visiting ROZE BioHealth Clinics in Dubai to experience biological dentistry firsthand and develop a personalized oral health strategy that supports your long-term wellness goals. Your mouth serves as the gateway to your health—make sure you’re protecting it with the care it deserves.